As part of our ongoing efforts to make high-quality and affordable healthcare available to our members, BCBSRI regularly reviews the list of prescription drugs we cover under our medical benefit. Our goal is to make sure that our members continue to have access to effective medications at the lowest possible cost. As a result, the following changes are being made to the medical drug review (MDR) program. Existing and new prior authorization reviews will continue to be handled by our pharmacy benefits manager, Prime Therapeutics.
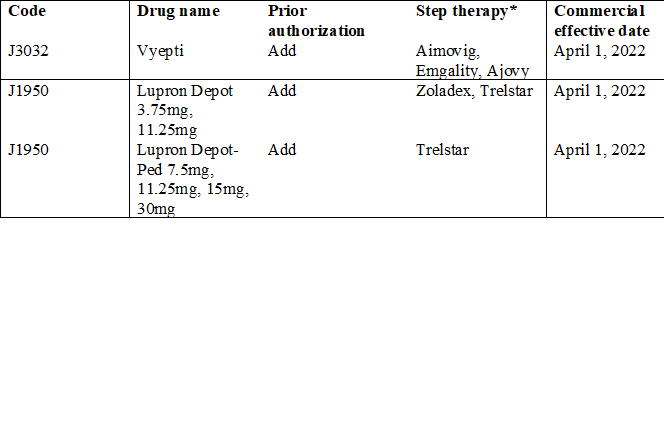
*Step therapy requires that specific drug(s) be used for treatment prior to another drug being allowed for coverage.
Please note the following Gonadotropin Releasing Hormone (GnRH) codes/drugs will continue to be covered WITHOUT requiring prior authorization:
J9217 Lupron Depot 7.5mg, 22.5mg, 30mg, 45mg
J9217 Eligard 7.5mg, 22.5mg, 30mg, 45mg
J3316 Trelstar 22.5mg
J9202 Zoladex 3.6mg, 10.8mg

